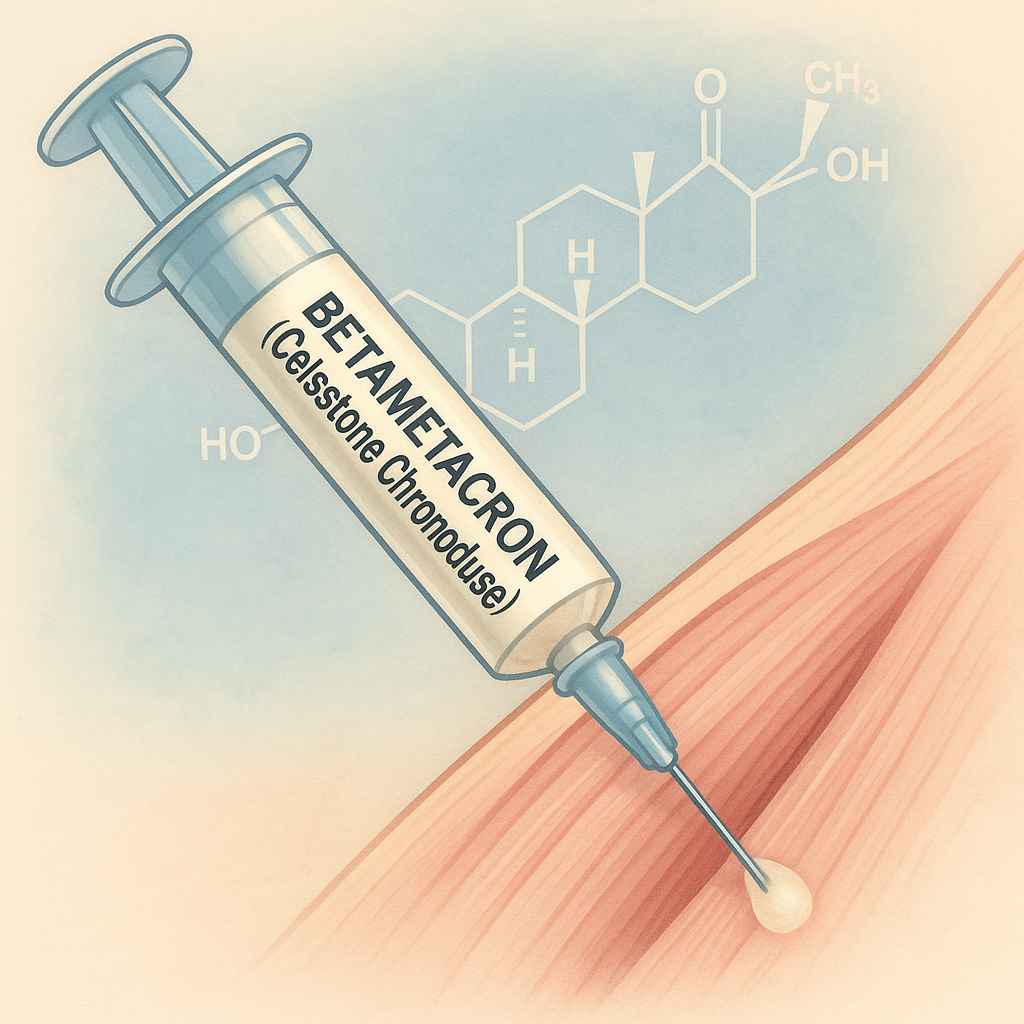
Women’s health often demands tailored therapeutic approaches that balance efficacy and safety, and few medications illustrate this balance better than Betametacron. Commonly known by its brand name Celestone Chronodose, Betametacron is an injectable, dual-ester formulation of the synthetic glucocorticoid betamethasone. Its unique design, combining a rapidly soluble phosphate ester for immediate onset with a slowly releasing acetate ester for sustained effect, renders it invaluable across a spectrum of inflammatory, autoimmune, allergic, and obstetric indications. From alleviating acute joint pain to promoting fetal lung maturity in preterm labor, Betametacron’s versatility has made it a cornerstone of modern corticosteroid therapy.
In this comprehensive article—written with a focus on women’s perspectives and concerns—we will explore Betametacron in depth. We will trace its pharmacological journey, dissect its mechanism of action, examine clinical uses and dosing strategies, and delve into safety considerations specific to women. We’ll also highlight key related terms to enhance online visibility, answer frequently asked questions, and discuss emerging research that may reshape its future role. Whether you are a healthcare professional, a patient navigating treatment options, or a health-conscious reader, this guide aims to empower you with clear, evidence-based insights.
What Is Betametacron?
Betametacron is the proprietary name for Celestone Chronodose, an aqueous suspension that contains two forms of betamethasone per milliliter:
-
Betamethasone sodium phosphate (3.9 mg): Water-soluble for rapid absorption and onset of action, typically within hours of intramuscular injection.
-
Betamethasone acetate (3 mg): Poorly soluble, creating a depot effect that slowly releases active drug over several days to a week.
This dual-ester approach ensures that patients receive both immediate anti-inflammatory relief and sustained control of symptoms from a single injection. Betametacron is approved for intramuscular, intra-articular, and intralesional administration when both prompt and prolonged corticosteroid activity are desired.
A Brief History of Corticosteroids and Betamethasone
The therapeutic era of corticosteroids began in the late 1940s, culminating in the 1950 Nobel Prize for Kendall, Reichstein, and Hench for isolating cortisone and demonstrating its efficacy in rheumatoid arthritis. Over the next decade, pharmaceutical chemists sought to enhance potency, stability, and specificity. In 1958, researchers at Schering synthesized betamethasone, distinguished by fluorination at the 9α position and methylation at the 16β position, yielding a molecule approximately 25 times more potent than cortisol with minimal mineralocorticoid activity.
Topical betamethasone formulations emerged in the early 1960s, rapidly becoming standard for dermatological conditions. By the 1970s, injectable esters—first the water-soluble sodium phosphate and later the prolonged-release acetate—were developed. In combining both esters into a single product, Celestone Chronodose (Betametacron) pioneered the convenience of dual-phase therapy, reducing the need for repeated injections and enabling clinicians to manage both acute flares and chronic inflammation with one dose.
Pharmacological Profile
Mechanism of Action
Betametacron exerts its effects by binding to cytoplasmic glucocorticoid receptors. The receptor–drug complex translocates to the nucleus, where it:
-
Upregulates anti-inflammatory proteins (e.g., lipocortin-1), which inhibit phospholipase A₂ and reduce arachidonic acid release.
-
Downregulates pro-inflammatory genes, decreasing the synthesis of interleukins (IL-1, IL-2, IL-6), tumor necrosis factor-alpha (TNF-α), and cyclooxygenase-2 (COX-2).
-
Stabilizes lysosomal membranes, preventing release of proteolytic enzymes.
-
Reduces capillary permeability, minimizing edema.
-
Suppresses leukocyte migration into inflamed tissues.
-
Inhibits fibroblast proliferation, slowing scar formation and collagen deposition.
These combined actions interrupt the inflammatory cascade at multiple levels, addressing both symptoms—redness, swelling, pain—and underlying immune activation.
Pharmacokinetics
-
Absorption: Following intramuscular injection, the sodium phosphate ester dissolves quickly, achieving peak plasma levels within 2–6 hours. The acetate ester forms a depot in muscle, releasing drug gradually over 5–10 days.
-
Distribution: Betamethasone is approximately 60–70% bound to plasma proteins, with widespread tissue distribution, including crossing the placenta and entering breast milk.
-
Metabolism: Primarily hepatic via CYP3A4 enzymes, generating inactive metabolites.
-
Elimination: Less than 5% of the dose is excreted unchanged in urine. The biological half-life varies: 36–54 hours for the sodium phosphate component and up to several days for the acetate component’s sustained release.
Formulations and Dosage Forms
Although Betametacron specifically denotes Celestone Chronodose, betamethasone itself appears in multiple formulations:
-
Injectable Suspensions
-
Celestone Chronodose (Betametacron): Dual-ester suspension, 5.7 mg/mL, for IM/intra-articular use.
-
Celestone Soluspan: Similar dual-ester with added preservatives.
-
-
Topical Preparations
-
Creams, Ointments, Gels, Lotions, Foams, Sprays: Betamethasone dipropionate or valerate at 0.05–0.1%. Potency ranges from medium to super-potent, depending on formulation and vehicle.
-
-
Oral Dosage
-
Tablets/Solution: Betamethasone 0.6 mg tablets or oral solutions (also combined with dexamethasone in some products) for systemic therapy in specific indications, though systemic side effects limit widespread oral use.
-
-
Ophthalmic Drops
-
Reserved for severe, non-infectious ocular inflammation due to risk of increased intraocular pressure and cataract formation.
-
Selecting the appropriate formulation depends on the target tissue, desired speed of onset, and duration of effect.
Clinical Indications
Betametacron’s versatility stems from its potent anti-inflammatory and immunosuppressive actions. Key indications include:
Rheumatological Disorders
-
Rheumatoid Arthritis: Intramuscular injections can abort acute flares when oral NSAIDs or DMARDs are insufficient.
-
Ankylosing Spondylitis & Psoriatic Arthritis: Provides rapid relief of spinal and peripheral joint inflammation.
-
Acute Gouty Arthritis: Single joint injections reduce pain and swelling when NSAIDs are contraindicated.
Dermatological Conditions
-
Severe Eczema & Psoriasis: Intralesional injections of Betametacron or high-potency topical betamethasone manage resistant plaques.
-
Bullous Dermatoses (e.g., Dermatitis Herpetiformis): Systemic corticosteroid injections can be life-saving in extensive, blistering skin disease.
-
Hypertrophic Scars & Keloids: Intralesional Betametacron disrupts fibroblast overactivity and collagen deposition, flattening raised lesions.
Allergic and Respiratory Disorders
-
Severe Asthma Exacerbations: IM Betametacron provides systemic control when inhaled therapy is inadequate or rapid systemic onset is preferred.
-
Allergic Rhinitis & Sinusitis: Systemic therapy for severe or refractory cases.
-
Drug Hypersensitivity Reactions: Attenuates systemic urticaria and angioedema.
Obstetric and Neonatal Applications
-
Fetal Lung Maturation: Two doses of 12 mg IM Betametacron given 24 hours apart to mothers at risk of preterm birth (< 32 weeks) reduce neonatal respiratory distress syndrome by up to 50%.
-
Prevention of Intraventricular Hemorrhage: Corticosteroids may reduce risk of brain bleeds in extremely preterm infants.
Autoimmune and Hematologic Conditions
-
Systemic Lupus Erythematosus Flares: Rapid control of life-threatening disease manifestations (e.g., lupus nephritis).
-
Immune Thrombocytopenia: Raises platelet counts by dampening autoantibody production.
-
Multiple Sclerosis Exacerbations: Short-course therapy for acute relapses.
Gastrointestinal Diseases
-
Inflammatory Bowel Disease: Injectable Betametacron used for Crohn’s disease and ulcerative colitis flares when oral steroids are not tolerated.
Ophthalmic Inflammation
-
Non-infectious Uveitis & Vitritis: Intra-vitreal injections can preserve vision in sight-threatening inflammation.
Dosage and Administration
Injectable Betametacron (Celestone Chronodose)
-
Adults:
-
Intramuscular (IM): 1–2 mL (5.7–11.4 mg) into a large muscle mass (e.g., gluteal).
-
Intra-articular: 0.5–2 mL per joint, depending on joint size.
-
Intralesional: 0.1–0.5 mL per cm² lesion.
-
-
Frequency: Doses may be repeated every 7–14 days as clinically indicated, not exceeding a cumulative dose that risks systemic toxicity.
-
Antenatal Use: Two 12 mg IM injections given 24 hours apart, ideally 48 hours before anticipated preterm delivery.
Topical Betamethasone
-
Apply a thin film once or twice daily to affected areas; limit continuous use to 14 days to avoid local atrophy and systemic absorption.
Oral Betamethasone
-
Dosage Range: 0.5–9 mg per day, divided into 2–4 doses; taper slowly over several weeks to months to prevent adrenal insufficiency.
Administration Tips
-
Proper Technique: Use a large-gauge needle (21–22 G) for IM injections; inject deeply into muscle and rotate sites.
-
Injection Site Care: Apply gentle pressure post-injection; avoid massaging to prevent depot disruption.
-
Storage: Keep vials refrigerated; bring to room temperature before use to minimize injection discomfort.
Safety Profile: Side Effects and Adverse Reactions
While highly effective, Betametacron carries a risk of both local and systemic adverse effects, especially with repeated or high-dose use.
Local Reactions
-
Injection Site Pain & Tenderness
-
Sterile Abscess Formation
-
Tissue Atrophy & Depigmentation
-
Skin Striae (with intralesional use)
Systemic Effects
Endocrine & Metabolic
-
Adrenal Suppression: Prolonged therapy downregulates the hypothalamic–pituitary–adrenal (HPA) axis.
-
Cushingoid Features: Moon face, buffalo hump, central obesity.
-
Hyperglycemia & New-Onset Diabetes
-
Fluid Retention & Hypertension
Musculoskeletal
-
Osteoporosis & Vertebral Compression Fractures
-
Proximal Muscle Weakness
Cardiovascular
-
Increased Thromboembolic Risk
-
Arrhythmias
Gastrointestinal
-
Peptic Ulcer Disease & GI Bleeding
-
Pancreatitis
Neuropsychiatric
-
Mood Swings, Insomnia, Depression, Psychosis
Ophthalmic
-
Cataract Formation
-
Glaucoma & Increased Intraocular Pressure
Mitigating Risks
-
Use the Lowest Effective Dose for the shortest duration.
-
Supplement Calcium & Vitamin D, consider bisphosphonates in long-term users.
-
Monitor blood pressure, blood glucose, bone density, and ocular pressure regularly.
-
Educate patients on recognizing early signs of infection, adrenal insufficiency, and psychiatric changes.
Drug Interactions
Betametacron’s systemic effects can be altered by numerous concomitant medications:
-
CYP3A4 Inducers (e.g., rifampin, phenytoin, carbamazepine): Accelerate metabolism, reduce efficacy.
-
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Combined use heightens risk of peptic ulcers.
-
Anticoagulants (e.g., warfarin): Variable effects on INR; necessitates close monitoring.
-
Diuretics: Potassium-wasting diuretics (loop, thiazide) increase hypokalemia risk.
-
Vaccines: Live attenuated vaccines contraindicated during high-dose corticosteroid therapy.
-
Antidiabetic Agents: May require dose adjustments due to hyperglycemic effects.
A thorough medication reconciliation and vigilant laboratory monitoring are essential whenever Betametacron is prescribed alongside interacting drugs.
You May Also Read: lg coco – malviya na: A Retro Revival for Feminine Simplicity in the Heart of Delhi
Special Considerations for Women
Pregnancy
-
FDA Category C: Animal studies reveal potential fetal harm; human data are limited.
-
Antenatal Use: Proven benefit for fetal lung maturation in preterm labor; two-dose regimen decreases neonatal respiratory distress without significant maternal harm.
-
Maternal Use: For non-obstetric indications, weigh benefits against risks—including possible fetal adrenal suppression and growth restriction.
Breastfeeding
-
Topical Betametacron poses minimal risk when used on non-breast areas.
-
Systemic therapy may transfer into breast milk; caution against prolonged high-dose use.
-
Recommend avoidance of application on or near nipples and advise on timing feeds relative to dosing.
Menstrual and Hormonal Effects
-
Corticosteroids can disrupt menstrual cycles and exacerbate conditions like polycystic ovary syndrome (PCOS) by altering glucose metabolism and androgen levels.
-
Monitor weight, blood pressure, and glucose tolerance in women with endocrine disorders.
Bone Health
-
Women are particularly susceptible to corticosteroid-induced osteoporosis.
-
Early initiation of bone-protective measures is crucial, especially in perimenopausal and postmenopausal patients.
Special Populations
Pediatrics
-
Pediatric dosing is weight-based (0.0175–0.25 mg/kg/day) with careful monitoring for growth suppression, adrenal axis suppression, and bone density.
Geriatrics
-
Increased sensitivity to side effects—osteopenia, hyperglycemia, hypertension.
-
Initiate at lower doses, monitor bone health, and optimize cardiovascular risk factors.
Comorbid Conditions
-
In patients with diabetes, adjust antidiabetic regimens to accommodate hyperglycemic effects.
-
In hypertensive or heart failure patients, monitor fluid status closely.
-
In those with peptic ulcer disease or gastrointestinal bleeding, co-prescribe gastroprotective agents (e.g., PPIs).
Patient Counseling and Monitoring
-
Explain the Purpose: Describe how Betametacron works and why the dual-ester formulation matters.
-
Review Administration: Proper IM injection technique, rotation of sites, and precautions.
-
Discuss Side Effects: Emphasize reporting of mood changes, vision disturbances, persistent GI pain, and signs of infection.
-
Tapering Plan: Outline the importance of gradual dose reduction to avoid adrenal crisis.
-
Routine Monitoring: Schedule labs for blood glucose, electrolytes, bone density scans, and eye exams.
-
Lifestyle Measures: Encourage calcium-rich diet, weight-bearing exercise, and smoking cessation to support bone health.
Frequently Asked Questions
-
How long does a single Betametacron injection last?
The sodium phosphate ester acts within hours and persists for 1–2 days, while the acetate ester provides anti-inflammatory effects for up to 7–10 days. -
Can Betametacron be used for chronic conditions?
Yes—repeat injections at intervals of at least one week can manage chronic flares, but consider transitioning to alternative maintenance therapies to minimize cumulative side effects. -
What should I do if I miss a dose?
For scheduled injections, contact your healthcare provider promptly. Do not double the next dose. -
Is Betametacron safe for children?
When dosed appropriately by weight and monitored closely for growth and adrenal function, Betametacron can be used in pediatric patients for severe inflammatory conditions. -
How is Betametacron different from prednisone?
Betametacron is more potent, has minimal mineralocorticoid activity, and the dual-ester formulation provides both immediate and prolonged effects, whereas prednisone is an oral corticosteroid requiring daily dosing.
Future Directions and Research
Recent investigations focus on Selective Glucocorticoid Receptor Modulators (SGRMs) derived from betamethasone analogues to retain anti-inflammatory benefits while reducing metabolic side effects. Clinical trials such as A*STEROID are comparing betamethasone with dexamethasone for antenatal use to refine safety profiles. Moreover, targeted intra-tumoral injections in oncology and nanoparticle-based delivery systems promise to localize drug action, minimizing systemic exposure.
Conclusion
Betametacron (Celestone Chronodose) exemplifies the evolution of corticosteroid therapy, marrying rapid relief with sustained control in a single injection. Its broad utility spans rheumatology, dermatology, allergy, obstetrics, and beyond, yet its potency necessitates judicious use—especially among women balancing reproductive health, bone integrity, and endocrine stability. By understanding its unique pharmacology, adhering to evidence-based dosing and monitoring, and integrating patient-centered counseling, healthcare providers can harness Betametacron’s therapeutic power while safeguarding quality of life.
Whether you are facing an acute inflammatory crisis or preparing for the arrival of a preterm infant, informed dialogue with your provider and personalized care plans will ensure that Betametacron serves as a valuable ally on your path to health.






Leave a Reply